
Washed microbiota transplantation targeting both gastrointestinal and extraintestinal symptoms in patients with irritable bowel syndrome
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder characterized by abdominal pain and changes in bowel habits. In addition to gastrointestinal symptoms, about 40% of patients with IBS also show a variety of extraintestinal symptoms, especially sleep disorders, anxiety and depression, which further impair their quality of life. However, there are few studies evaluating the efficacy of fecal microbiota transplantation for gastrointestinal symptoms and extraintestinal symptoms in patients with IBS. Recently, “Progress in Neuropsychopharmacology & Biological Psychiatry” published a clinical study from our team entitled “Washed microbiota transplantation targeting both gastrointestinal and extraintestinal symptoms in patients with irritable bowel syndrome”. This study evaluated the efficacy of washed microbiota transplantation (WMT) on gastrointestinal symptoms and psychological symptoms (sleep, anxiety, depression) in patients with IBS, and focused on the change of sleep quality and its influencing factors.
Methods: This was a prospective observational study involving patients with IBS who underwent WMT at the Second Affiliated Hospital of Nanjing Medical University from October 2020 to September 2022. The Pittsburgh Sleep Quality Index (PSQI) was used to assess sleep quality. The Gastrointestinal Symptom Rating Scale (GSRS) and IBS Severity Scoring System (IBS-SSS) were used to evaluate gastrointestinal symptoms and IBS severity, respectively. The Self-rating Depression Scale (SDS) and Self-rating Anxiety Scale (SAS) were used to evaluate depression and anxiety, respectively. All the symptoms were evaluated at baseline and one month after WMT. A multiple logistic regression model was used to determine the predictive factors of sleep improvement one month after WMT.
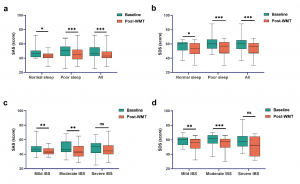
The efficacy of WMT in patients with IBS
A significant decrease in IBS-SSS and GSRS scores was observed in all patients (IBS-SSS: Z = −6.468, P < 0.001; GSRS: Z = −5.364, P < 0.001; Fig. 1a, b) and patients with poor sleep quality one month after WMT (IBS-SSS: t = 8.188, P < 0.001; GSRS: t = 5.933, P < 0.001; Fig. 1a, b). WMT decreased IBS-SSS and GSRS scores from the baseline in patients with moderate IBS (IBS-SSS: t = 10.215, P < 0.001; GSRS: t = 5.704, P < 0.001) and severe IBS (IBS-SSS: t = 4.168, P = 0.002; GSRS: t = 2.732, P = 0.019).
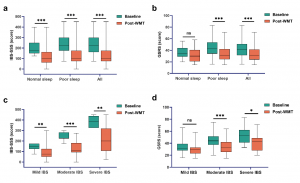
WMT ameliorated psychological symptoms in patients with IBS
There was a statistically significant reduction in SAS and SDS scores one month after WMT regardless of their baseline sleep quality (normal sleep: SAS: Z = −2.560, P = 0.010; SDS: t = 2.173, P = 0.042; poor sleep: SAS: t = 4.079, P < 0.001; SDS: Z = −4.070, P < 0.001; all patients: SAS: Z = −4.775, P < 0.001; SDS: Z = −4.610, P < 0.001; Fig. 2a, b). However, anxiety and depression alleviation was only observed in patients with mild (SAS: t = 3.426, P = 0.002; SDS: t = 3.148, P = 0.004; Fig. 2c, d) and moderate IBS symptoms (SAS: t = 3.400, P = 0.002; SDS: t = 4.180, P < 0.001; Fig. 2c, d) one month after WMT.
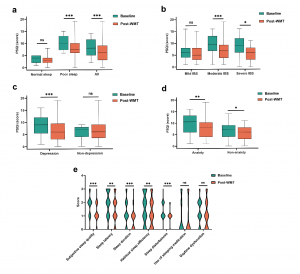
WMT alleviated sleep disturbances in patients with IBS
Patients with moderate and severe IBS experienced a significant reduction in PSQI scores (moderate IBS: t = 4.065, P < 0.001; severe IBS: t = 2.664, P = 0.022; Fig. 3b). Relief from sleep disturbances after WMT was observed independent of anxiety status (patients with anxiety: Z = −3.210, P = 0.001; patients without anxiety: Z = −2.534, P = 0.011; Fig. 3d). The five components of PSQI in patients with poor sleep quality also improved one month after WMT compared to baseline scores: subjective sleep quality (Z = −4.259, P < 0.001), sleep latency (Z = −3.427, P = 0.001), sleep duration (Z = −4.075, P < 0.001), habitual sleep efficiency (Z = −2.643, P = 0.008) and sleep disturbances (Z = −3.500, P < 0.001) (Fig. 3e).
This study provided real-world study evidence that WMT effectively improved both gastrointestinal and extraintestinal symptoms in patients with IBS. Clinicians and researchers can be encouraged to perform WMT to optimize the management of IBS and other microbiota-gut-brain-axis-related diseases. The present study suggests a more significant implication that patients diagnosed with traditional IBS may potentially have an underlying dysbiosis, leading to organ damage that is not discernible through conventional diagnostic criteria. These findings may shed light on the reasons why certain individuals with IBS benefited from WMT. In essence, our research provides compelling evidence that challenges the prevailing concept of IBS.


